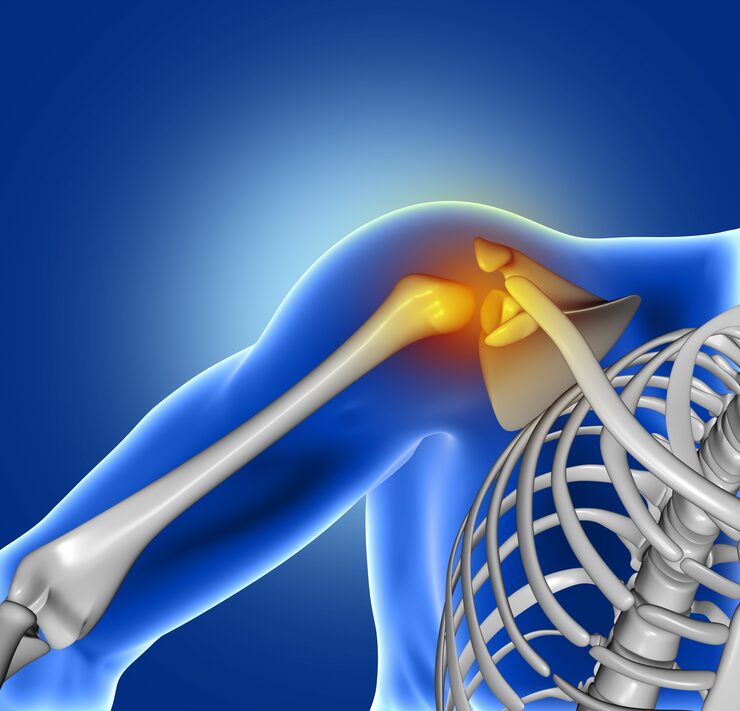
visual representation of osteonecrosis
Bones are living tissues that get new blood all the time, which keeps them healthy. When this blood supply stops, though, bone tissue can start to die, which can cause a painful and possibly crippling condition called osteonecrosis, or avascular necrosis (AVN).
Osteonecrosis can happen to anyone; however, it happens more often to adults between the ages of 30 and 60. Early diagnosis and treatment are crucial for preventing joint collapse and maintaining mobility.
In this blog, we'll talk about what osteonecrosis is, what causes it, how to tell if you have it, how to diagnose it, and the different ways to treat it to improve your bone health and quality of life.
The word "osteonecrosis" implies "death of bone." When a part of the bone loses its blood supply, the bone tissue weakens, collapses, and eventually breaks down.
If this happens near a joint, the smooth cartilage that covers the bone surface may also break down, which can cause arthritis and render the joint ineffective.
The disorder can affect any bone; however, it most often affects the:
When blood flow to a bone is cut off or slowed, osteonecrosis occurs. There are several things that can get in the way of this circulation:
A fracture or dislocation may damage the blood vessels that supply blood to the bone. This is a common reason why people develop osteonecrosis of the hip after a hip fracture.
Taking a lot of corticosteroid drugs (like prednisone) for a long time can cause fat to build up in blood vessels, which makes it harder for blood to flow to the bone.
Alcohol can cause fat to build up in the blood arteries, which can make it harder for blood to flow to the bones.
These cancer treatments can hurt blood arteries, which makes bone necrosis more likely.
Idiopathic osteonecrosis occurs when no definite etiology can be found.
Osteonecrosis can affect everyone; however, some groups are more likely to get it than others, such as:

old person experiencing pain due to osteonecrosis
Osteonecrosis typically begins with mild symptoms that worsen over time. As the condition gets worse, the symptoms can become very bad and make it hard to do everyday things.
In the Early Stages (Before the Bone Breaks):
Progressive Stages: Pain that doesn't go away and gets worse even when you're not moving
Finding it early is crucial to prevent damage to the joints. To determine if someone has osteonecrosis, doctors review their medical history, perform imaging tests, and conduct a clinical examination.
1. A physical exam and a history
Your doctor will look at your symptoms, medical history, and any risk factors you may have, such as using steroids, drinking alcohol, or having had injuries in the past.
2. Imaging Tests X-rays: Changes may not show up in the early stages, but later pictures can show bone collapse or joint deformity.
MRI (Magnetic Resonance Imaging): The most accurate test for finding problems early on. It can detect osteonecrosis before the symptoms worsen.
CT scans provide detailed images of your bones and joints, allowing you to assess the extent of the damage.
Bone scans may help find changes in blood flow and bone activity.
3. Tests on blood
Even though they don't tell you what's wrong, they might help you find out if you have lupus or sickle cell disease.
Depending on how bad the bone degeneration is, doctors usually divide osteonecrosis into four stages:
Stage I: X-rays are normal, but the MRI reveals reduced blood flow.
Stage II: X-rays show early alterations in the bones, but the joint surface is still fine.
Stage III: The bone begins to break down, resulting in joint problems
Stage IV: There is a lot of arthritis and joint deformities.
Early diagnosis provides the best opportunity for recovery without surgery.
The goal of treatment is to prevent further bone breakdown and maintain joint function. The stage of the disease, the affected bone, and the patient's overall condition all play a role in determining a treatment.
1. Non-Surgical Treatments (Early Stages) Medications:
Some therapies utilize electrical currents to aid in bone development and healing.
2. Surgery (for advanced stages)
If the bone has already broken or conservative techniques are not effective, surgery may be necessary to restore joint function.
Some common types of surgery are:
Core Decompression: A small piece of bone is removed to ease pressure, enhance blood flow, and accelerate healing. Frequently employed in the initial phase of hip osteonecrosis.
Bone Grafting: To repair damaged bone, healthy bone tissue is transferred from another part of the body or from a donor.
Osteotomy: The bone is manipulated to shift weight away from the injured location, which can help delay the need for joint replacement.
Arthroplasty, or joint replacement, involves the placement of an artificial implant in a damaged joint to restore movement and alleviate pain. The most prevalent types of replacements are for the hips and knees.
Osteonecrosis can cause: Complete bone collapse if not addressed

doctor explaining osteonecrosis
Even though osteonecrosis can't always be stopped, you can lower your risk by doing specific things:
If you have joint pain, stiffness, or trouble walking that you can't explain, especially after an injury or while using corticosteroid medicine, you should see an orthopedic specialist right away. The best way to avoid permanent bone damage is to receive treatment as soon as possible.
Osteonecrosis is a dangerous disorder, but it can be treated. Patients can often regain their mobility and live pain-free lives if they are diagnosed and treated promptly, with the right medications, lifestyle adjustments, and even modern surgical interventions when necessary.
Our orthopedic surgeons, rehabilitation specialists, and radiologists at [Hospital Name] collaborate to treat a wide range of bone and joint conditions, including osteonecrosis. We help patients recover faster and feel better about returning to their daily activities by utilizing modern imaging, minimally invasive surgery, and individualized rehabilitation programs.
Call today to schedule a consultation if you have joint discomfort that won't go away or if you are at risk for osteonecrosis. Getting help early can make a significant difference in maintaining your joint health and maintaining a high quality of life.
We offer expert care across key specialties, including Medicine, Cardiology, Orthopaedics, ENT, Gynaecology, and more—delivering trusted treatment under one roof.

Dr. R.C. Sharma

Dr. Rakesh

Dr. Alka Kapoor
Prakash Hospital Pvt. Ltd. is a 100 bedded NABH NABL accredited multispecialty hospital along with a center of trauma and orthopedics. We are in the service of society since 2001.
OUR SPECIALITIES
Contact Us
D – 12A, 12B, Sector-33, G. B. Nagar, Noida, Uttar Pradesh 201301
+91-8826000033

© 2026 All rights reserved.
Designed and Developed by Zarle Infotech