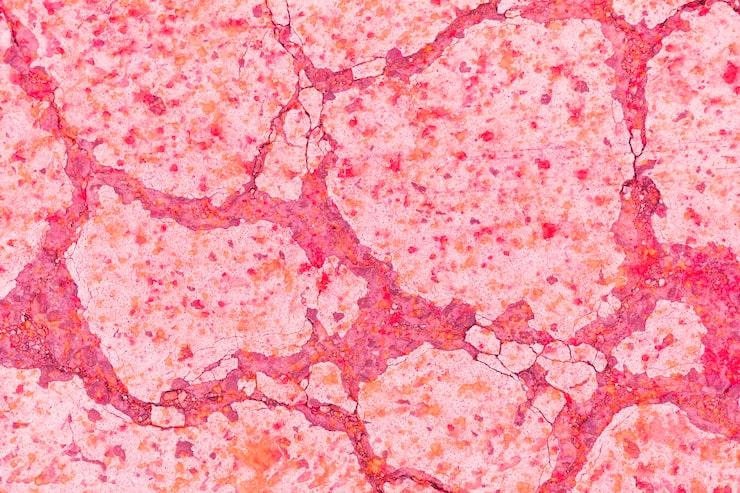
tissues under a microscope
Blood flow constantly supplies oxygen and nutrients to healthy tissue. When this flow is halted or hurt, cells start to die. This is called necrosis of tissue.
Tissue necrosis is not a disease in itself; it is a severe side effect of other diseases that cause or disrupt blood flow. It can happen in the skin, muscles, bones, or organs inside the body. If you don't obtain medical assistance right away, it could grow infected, develop gangrene, or even have to be cut off.
At Prakash Hospital in Noida, our full team of specialists offers contemporary wound treatment and surgery for patients with tissue necrosis. Knowing what the condition is and its signs can help you receive medical attention sooner and avoid complications.
Tissue necrosis is the death of body tissue caused by a lack of blood flow, a serious sickness, an injury, or exposure to chemicals. Cells die and make enzymes that damage neighboring healthy tissues when they don't get enough oxygen and nutrients.
Natural cell death is controlled and doesn't injure surrounding tissue, whereas necrosis is uncontrolled and typically causes inflammation, swelling, and tissue collapse.
Black, hard, or discolored skin can be a sign of necrosis, and it can worsen quickly if an infection occurs. That's why it's crucial to identify and treat it early.
Doctors categorize necrosis according to its impact on tissue. Some common types are: 1. Coagulative necrosis happens when the blood supply is cut off (ischemia).
These are often detected in the heart, kidneys, and liver.
The affected area appears pale and firm.
2. Necrosis that becomes liquid
Characterized by tissue that is liquid or pus-like, usually because of a bacterial infection.
Common in brain tissue and abscesses.
3. Necrosis of the caseous kind
Seen in diseases like TB, where the tissue looks mushy and "cheesy."
4. Death of Fat
This occurs when fat cells are damaged, typically in the pancreas or breast, due to an injury or inflammation.
5. Gangrenous Necrosis: This is a highly serious and advanced type of necrosis that arises when blood flow is cut off for a long time or an infection occurs.
When an infection arises, this is called wet gangrene. When there is no infection, the condition is referred to as dry gangrene.

a model of dead tissue
When cells don't receive enough oxygen or are directly harmed, tissue necrosis occurs.
Here are some common reasons:
At Prakash Hospital, we focus on identifying risks early by conducting comprehensive screenings on patients with diabetes, vascular disease, or mobility issues.
Seeing the first indicators helps prevent tissue damage from worsening.
Some common warning indicators are:
If you notice these indicators, especially after an injury or surgery, consider visiting Prakash Hospital in Noida, which is quite a distance away.
Our physicians at Prakash Hospital utilize cutting-edge diagnostic technologies to determine the extent of necrosis and its underlying cause.
Some ways to diagnose are:
Early diagnosis helps figure out if the tissue can be saved or needs to be cut out.

doctor taking care of the patient
The goal of the treatment plan is to stop tissue death, get rid of dead tissue, control infection, and get circulation flowing again.
1. Drugs
Antibiotics to stop infections.
Painkillers and anti-inflammatory medicines to help with symptoms.
Anticoagulants help blood flow and stop clots from forming.
2. Cleaning and caring for wounds
Wound care specialists change sterile dressings, clean wounds, and keep an eye on them.
Safe removal of dead tissue using surgery or enzymes.
Negative Pressure Wound Therapy (NPWT) is a vacuum-assisted method that speeds up healing.
3. Hyperbaric Oxygen Therapy (HBOT)
Patients breathe 100% oxygen in a chamber with higher pressure, which helps get more oxygen to damaged tissues and speeds up healing.
4. Management by surgery
Reconstructive surgery or skin grafting makes tissue look and work better
Amputation is not common, although it may be necessary in severe gangrene to stop the infection from spreading.
5. Bettering blood flow
Angioplasty or bypass surgery may be done to open up clogged arteries and let blood flow again.
6. Food and recovery
Eating a lot of protein and vitamins helps you heal.
Physiotherapy can help strengthen weak areas and enhance blood flow.
Patients at Prakash Hospital's Advanced Wound Care Unit get personalized treatment programs that include medical treatments, surgery, and nutritional advice to help them fully recover.
Most people who have tissue necrosis get better with early diagnosis and professional therapy. How quickly the illness is treated and how much tissue is impacted will affect the prognosis.
To fully recover, you must follow the doctor's recommendations, eat well, and go to all of your follow-up appointments.
At Prakash Hospital, our skilled team of vascular surgeons, wound care specialists, plastic surgeons, and infection control experts works together to fully address tissue necrosis.
We help patients heal quickly and feel better by using the most up-to-date diagnostic imaging, hyperbaric oxygen therapy, innovative debridement techniques, and tailored wound care.
If you see that your skin is changing color, your wounds are taking a long time to heal, or you have a bad-smelling discharge, don't wait—go to Prakash Hospital in Noida right away for a quick check-up and treatment.
Because early intervention saves tissue and lives, your health and recovery are our top concerns.
We offer expert care across key specialties, including Medicine, Cardiology, Orthopaedics, ENT, Gynaecology, and more—delivering trusted treatment under one roof.
Prakash Hospital Pvt. Ltd. is a 100 bedded NABH NABL accredited multispecialty hospital along with a center of trauma and orthopedics. We are in the service of society since 2001.
OUR SPECIALITIES
Contact Us
D – 12A, 12B, Sector-33, G. B. Nagar, Noida, Uttar Pradesh 201301
+91-8826000033

© 2026 All rights reserved.
Designed and Developed by Zarle Infotech